Bionic Eyes: Navigating the Frontier of Vision Restoration

Read time: 4 minutes
The future is now. Let’s explore some insights into bionic eyes, a groundbreaking field that seeks to restore vision using advanced technological solutions, and the potential they hold for revolutionizing the way we perceive the world.
Bionic eyes, also called retinal implants or visual prosthetics, represent a new approach to treating profound vision impairment. These devices are designed to bypass damaged parts of the visual system and provide a form of artificial vision.
The Landscape of Vision Impairment
To understand the significance of bionic eyes, it's essential to first appreciate the challenges faced by individuals with severe vision impairment.
Vision impairment can arise from diverse factors, including retinal diseases, optic nerve damage, and certain genetic conditions. Conventional treatments have limitations in addressing severe cases, leaving many individuals with limited options for vision restoration.
The Emergence of Bionic Eyes
Bionic eyes, also known as retinal implants or visual prosthetics, represent a revolutionary approach to vision restoration. These devices are designed to bypass damaged or non-functional parts of the visual system, providing individuals with a form of artificial vision.
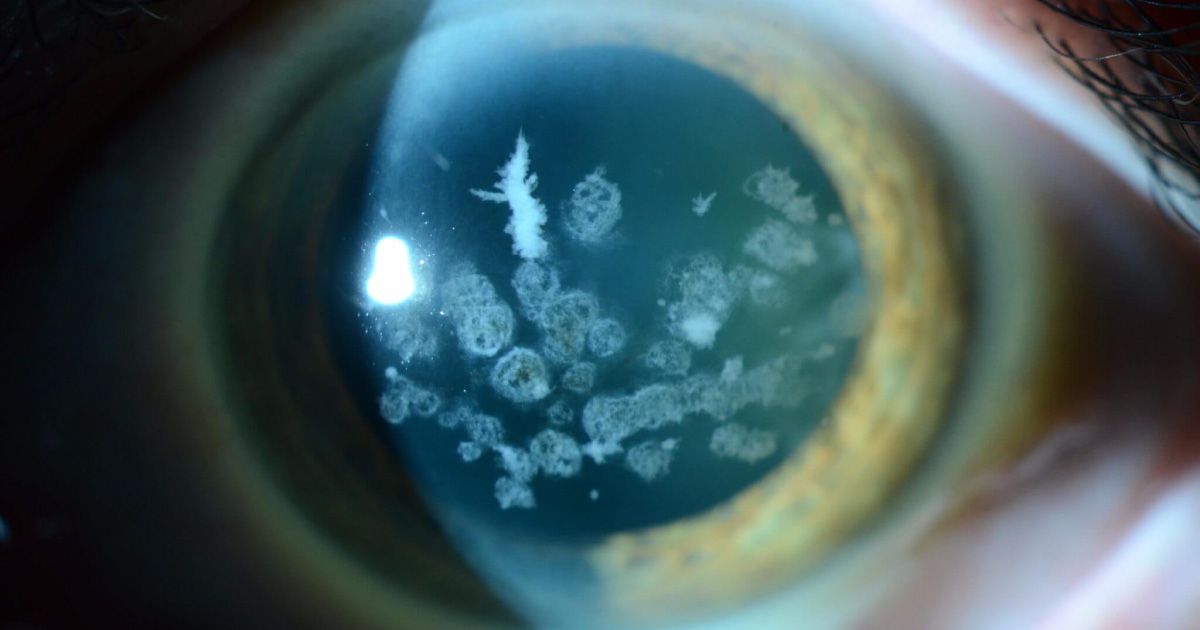
The core technology behind bionic eyes involves implanting microelectrode arrays into the retina or the visual cortex of the brain. These electrodes stimulate the remaining healthy cells, effectively bypassing damaged photoreceptor cells in the case of retinal implants or damaged optic nerve fibers in the case of cortical implants. This stimulation helps to create visual signals the brain can interpret.
Types of Bionic Eyes
There are currently two main types of bionic eyes in development, each addressing different aspects of vision impairment. This section provides an overview of retinal implants and cortical implants, detailing their mechanisms and potential applications.
- Retinal Implants: Retinal implants focus on stimulating the remaining functional cells in the retina, aiming to restore some level of vision for individuals with retinal diseases. These devices convert visual information captured by a camera into electrical signals that the brain can interpret.
- Cortical Implants: Cortical implants, on the other hand, target the visual cortex of the brain. By directly stimulating this area, these implants seek to provide artificial vision for individuals with optic nerve damage or other conditions affecting the visual pathways.
The Journey of Bionic Eye Recipients
- Patient Selection and Evaluation: The process of receiving a bionic eye involves a thorough evaluation to determine the suitability of the individual for the technology. Factors such as the cause of vision loss, overall eye health, and the specific type of implant are carefully considered.
- Surgical Implantation: The surgical procedure for implanting a bionic eye is a delicate and intricate process. Surgeons work to secure the microelectrode array in the designated area, ensuring optimal placement for effective stimulation of the visual system.
- Post-Implant Rehabilitation: Following implantation, recipients undergo a period of rehabilitation to adapt to the artificial vision provided by the bionic eye. This phase involves learning to interpret the visual signals generated by the device and integrating this newfound vision into daily life.
Real-World Impact and Limitations
Bionic eyes have shown promise in restoring a degree of independence to individuals with profound vision impairment. Recipients report improvements in tasks such as recognizing faces, navigating environments, and engaging in activities that were once challenging or impossible.
While bionic eyes represent a significant leap forward, they are not without limitations. Factors such as the resolution of artificial vision, the complexity of the surgical procedure, and the need for ongoing research and development present challenges to widespread adoption.
The Future of Bionic Eyes
- Ongoing Research and Advancements: The field of bionic eyes is dynamic, with ongoing research aiming to enhance the technology's capabilities. Scientists and engineers are exploring ways to improve the resolution of artificial vision, expand the range of visual stimuli, and address the diverse causes of vision impairment.
- Potential Applications Beyond Vision Restoration: The impact of bionic eyes extends beyond vision restoration. Researchers are exploring potential applications in enhancing natural vision, improving perception in low-light conditions, and even incorporating additional features such as augmented reality.
The Takeaway
Bionic eyes represent a monumental stride in vision restoration, offering hope and possibilities for individuals facing profound vision impairment. While still in its early stages, this technology holds immense potential to transform the lives of millions living with vision loss. As research progresses and breakthroughs are made, we can expect bionic eyes to become more sophisticated, affordable, and accessible. The future of vision restoration is bright, and bionic eyes are poised to play a pivotal role in illuminating the path towards a world where everyone can experience the wonder of sight.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.