Retinal Detachment Warning Signs to Look Out For
Read time: 5 minutes
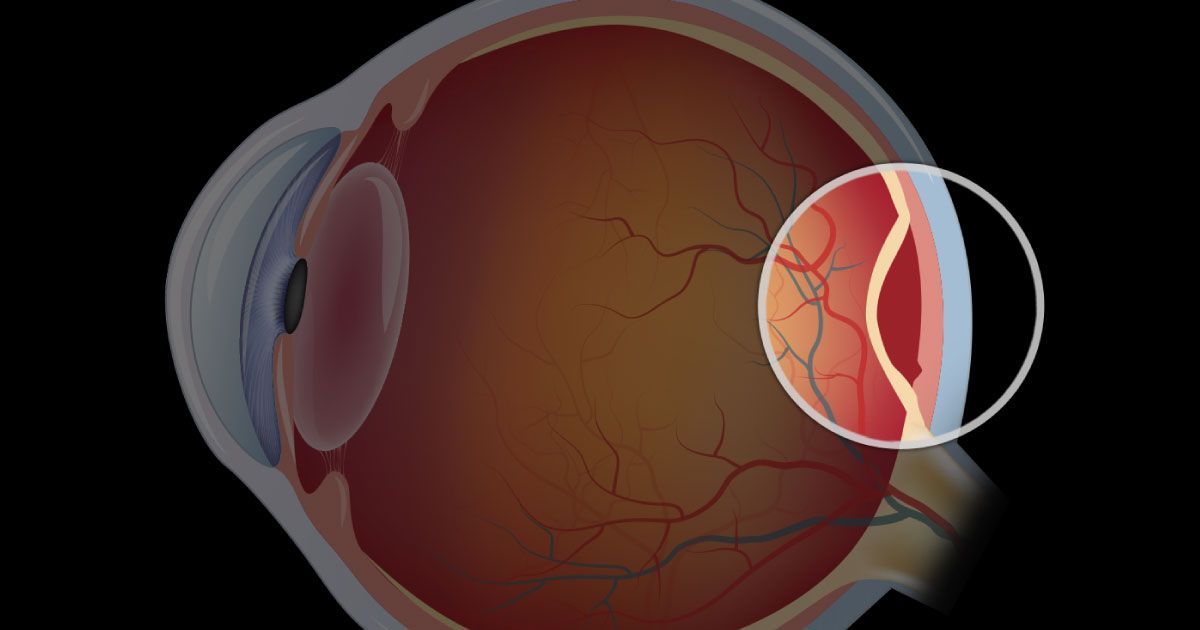
Retinal detachment is a serious condition that can lead to vision loss if not treated quickly. It's important to know the warning signs so you can seek help right away. The retina is a thin layer of tissue at the back of the eye that helps us see. When the retina detaches, it pulls away from its normal position, which can cause permanent damage.
Imagine your eye is like a camera. The retina acts like the film or digital sensor that captures the images we see. If the retina is damaged or out of place, the camera can't take clear pictures. This is why recognizing the signs of retinal detachment early is so important. Quick treatment can make a big difference in saving your vision.
In this article, we will look at the key warning signs of retinal detachment, why it's urgent to seek treatment, and the medical solutions available to help protect your vision. Understanding these signs can help you and your loved ones keep your eyes healthy and your vision clear.
What Is Retinal Detachment?
Retinal detachment happens when the retina, a thin layer of tissue in the back of the eye, separates from its normal position. The retina is crucial because it sends visual information to the brain. If it detaches, the retina can no longer function properly, leading to serious vision problems.
The eye is similar to a camera. The retina acts like the film or the digital sensor that captures the images we see. When the retina detaches, it's like removing the film from a camera, making it impossible to take a clear picture. Understanding the role of the retina helps highlight why quick action is essential if detachment occurs.
Key Warning Signs of Retinal Detachment
Recognizing the early signs of retinal detachment is vital to protect your vision. There are a few key symptoms to watch for:
- Sudden Appearance of Floaters: These are tiny specks or strings that drift into your field of vision. They can be a sign of changes in the eye that might lead to retinal detachment.
- Flashes of Light in Peripheral Vision: Seeing flashes of light, especially in the side vision, can indicate that the retina is under stress and pulling away from its normal position.
- Shadow or Curtain Effect Over Vision: You might notice a dark shadow or curtain moving across your vision. This effect can start in one area and spread, indicating that the retina may be detaching.
These warning signs should never be ignored. If you experience any of these symptoms, seek medical attention immediately to prevent permanent vision loss.
To learn more about the types of sudden vision changes and their symptoms, read our article Decoding Sudden Vision Changes
The Urgency of Seeking Treatment
Seeking treatment for retinal detachment as soon as warning signs appear is crucial. Delay can lead to severe consequences, including permanent loss of vision. The longer the retina remains detached, the greater the risk of irreversible damage.
Delaying treatment can result in permanent vision loss, including blindness in the affected eye. Additionally, the longer the retina stays detached, the more complex and risky any potential surgery can become. Early intervention greatly reduces these complications and improves the likelihood of successful outcomes.
Importance of Early Detection for Preserving Vision
Early detection plays a vital role in the success of treatment. Immediate attention can significantly improve the chances of saving your vision. Identifying and addressing retinal detachment quickly helps prevent further complications and enhances the effectiveness of medical interventions.
What to Do If You Experience Symptoms
If you notice any warning signs such as floaters, flashes, or a shadow over your vision, it’s essential to contact an eye specialist immediately. Avoid delaying care or waiting to see if symptoms improve on their own. Prompt medical attention is critical for achieving the best possible outcome.
- Medical Solutions and Treatments: There are several treatments available for retinal detachment, and the best approach depends on the severity and specific nature of the condition. Eye care professionals will assess the situation and recommend an appropriate treatment plan to preserve and restore vision.
- Common Surgical Procedures: Scleral buckle surgery involves placing a silicone band around the eye to push the wall of the eye against the detached retina. Another common procedure is vitrectomy, where the vitreous gel pulling on the retina is removed and replaced with a gas bubble to help reattach the retina.
- Laser Therapy Options: Laser photocoagulation uses a focused laser to create small burns around the retinal tear, helping to seal the retina back in place. Cryopexy is another method where a freezing probe is used to create scar tissue that secures the retina and prevents further detachment.
- Recovery and Follow-Up Care: After surgery, following your doctor’s instructions carefully is essential for proper healing. Regular eye exams should be scheduled to monitor the health of your retina and catch any potential issues early. You may also need to follow temporary activity restrictions, such as avoiding heavy lifting or sudden movements, to protect your recovery and ensure optimal results.
The Takeaway
Retinal detachment is a serious condition that requires immediate attention. Understanding the key warning signs, such as sudden floaters, flashes of light, and a curtain effect over your vision, is crucial. Early detection and treatment can save your vision and prevent permanent damage.
If you experience any symptoms of retinal detachment, contact your local emergency eye care facility so you can be seen immediately. If your eye injury or emergency occurs after hours and you are unable to reach an open facility, seek help at the nearest hospital emergency room, or call 911.
Always seek emergency care if you believe your eyesight is in jeopardy or if you are in severe pain.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.


















