Stargardt Disease: A Clearer Look at Juvenile Macular Dystrophy

Read time: 5 minutes
The eye is one of the body’s most remarkable organs, capable of capturing fine detail and vibrant color. But it’s also vulnerable to conditions that can impair vision. One such disorder is Stargardt disease, the most common form of inherited macular dystrophy. Though relatively rare, it affects thousands of people worldwide and often begins in childhood or adolescence.
What Is Stargardt Disease?
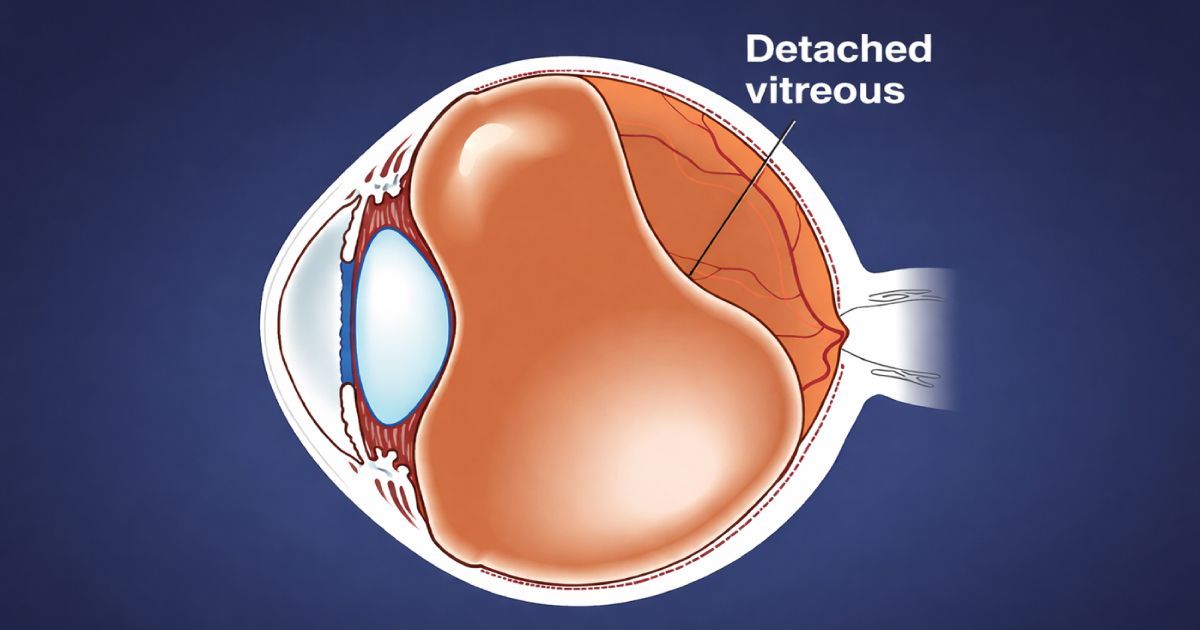
Stargardt Disease, also called juvenile macular dystrophy, is the most common inherited form of macular degeneration. It affects the macula — the central part of the retina responsible for sharp, detailed vision — and typically begins in childhood or adolescence. According to the National Eye Institute, the condition is caused by mutations in the ABCA4 gene, leading to a buildup of toxic fatty deposits in the retina that gradually damage central vision.
Patients with Stargardt disease typically experience a loss of clarity in their central vision but often retain peripheral vision, which helps them move around and stay independent.
A Short History
The condition was first described in 1909 by German ophthalmologist Karl Stargardt, who noted a distinct pattern of vision loss and retinal changes in younger patients. Since then, advances in imaging and genetics have revealed the underlying mechanisms he first observed more than a century ago.
Common Symptoms
Because the cornea and macula are so sensitive, early changes in Stargardt disease are often noticeable. Symptoms include:
- Blurry or distorted central vision
- Dark or blank spots in the middle of vision
- Difficulty reading or recognizing faces
- Light sensitivity
- Changes in color perception
The first signs usually appear in childhood, the teen years, or early adulthood. Symptoms may worsen slowly over time, though the rate of progression varies widely.
Who Gets Stargardt Disease?
Stargardt disease is inherited in an autosomal recessive pattern. This means both parents typically carry one copy of the faulty gene without showing symptoms. When a child inherits two copies, one from each parent, the disease develops.
It is estimated to affect 1 in 8,000 to 10,000 people worldwide, making it uncommon but not exceptionally rare.
Progression and Daily Life
The course of Stargardt disease differs from person to person. Some notice vision loss early and progress quickly, while others retain useful sight for decades. Complete blindness is rare, as peripheral vision often remains intact.
Adapting to vision changes is key. Patients often use:
- Magnifiers or digital readers for text
- High-contrast settings on electronic devices
- Tinted or polarized lenses to reduce glare
- Low vision rehabilitation to support independence
Beyond tools, emotional support and counseling can make a major difference in adapting to changes and staying confident.
Current Research and Emerging Treatments
While there’s no cure yet, exciting advances are underway:
- Gene therapy is being tested to deliver a healthy copy of the ABCA4 gene to retinal cells.
- Stem cell therapy aims to replace damaged retinal cells.
- Drug therapies are in development to slow the buildup of toxic byproducts.
- Light management strategies encourage patients to wear UV-blocking eyewear, as sunlight may worsen retinal damage.
These approaches are at different stages of research, but they offer growing hope for treatments that could slow or even halt the disease’s progression.
Organizations like the Foundation Fighting Blindness are leading efforts to fund research, provide patient resources, and connect families with emerging treatment opportunities.
The Outlook
A diagnosis of Stargardt disease can feel overwhelming, especially when it happens in childhood. But with today’s low vision technology, support systems, and ongoing research, patients can continue to live full and active lives.
From Karl Stargardt’s first observations in 1909 to today’s genetic research, the journey has been one of persistence and progress. And with clinical trials advancing, the future looks more promising than ever.
The Takeaway
Stargardt disease is the most common inherited form of macular dystrophy, typically beginning in youth and leading to gradual central vision loss. While no cure exists yet, support tools and groundbreaking research are making a meaningful impact on patient care.
For those living with the condition, early diagnosis, lifestyle adjustments, and staying connected with an eye care provider can help protect remaining vision and maintain quality of life.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.