Visual Snow Syndrome: The Static You Can't Turn Off

Read time: 7 minutes
Imagine looking at the world, but instead of seeing it clearly, it's covered by a constant shimmer of tiny, flickering dots, like static on an old TV screen. This isn't just a trick of the light or tired eyes; it's a real and confusing condition called Visual Snow Syndrome (VSS). For people with VSS, this "static" is always there, no matter what they're looking at or how bright the room is.
For a long time, doctors didn't fully understand VSS. People who saw this persistent static often felt alone, and their vision problems were sometimes mistakenly called anxiety or other mental health issues, especially since their regular eye exams showed nothing wrong. But now, thanks to more research, we're finally starting to understand this mysterious neurological condition.
The History of Understanding VSS
It took many years for Visual Snow Syndrome to be officially recognized in the medical world. While people have likely experienced it for centuries, it wasn't until recently that doctors had a name and understanding for it. One of the earliest medical reports about seeing "snowy vision" came in 1944, when a doctor named Frank D. Carroll described patients with these ongoing visual disturbances and thought it might be a problem with the brain.
Later, an important study in 1995 provided more clear descriptions of patients who saw continuous visual static. At first, this was thought to be just a type of migraine, but over time, it became clear that VSS was its own separate condition with a wider range of symptoms. Between 2012 and 2014, key researchers like Dr. Peter Goadsby and Dr. Christoph Schankin played a crucial role in defining VSS and setting up clear rules for diagnosing it. This was a huge step, moving VSS from being seen as a mental issue to a real neurological problem.
In recent years, groups like the Visual Snow Initiative have pushed for even more research, greatly improving our understanding. Brain scans now clearly show that people with VSS have differences in how certain parts of their brain work, proving that VSS isn't an eye problem, but a brain problem. A significant milestone occurred in 2024-2025, when the World Health Organization officially gave VSS its own medical codes (ICD codes). This monumental step signifies that VSS is now globally recognized by doctors everywhere.
What Causes the Static?
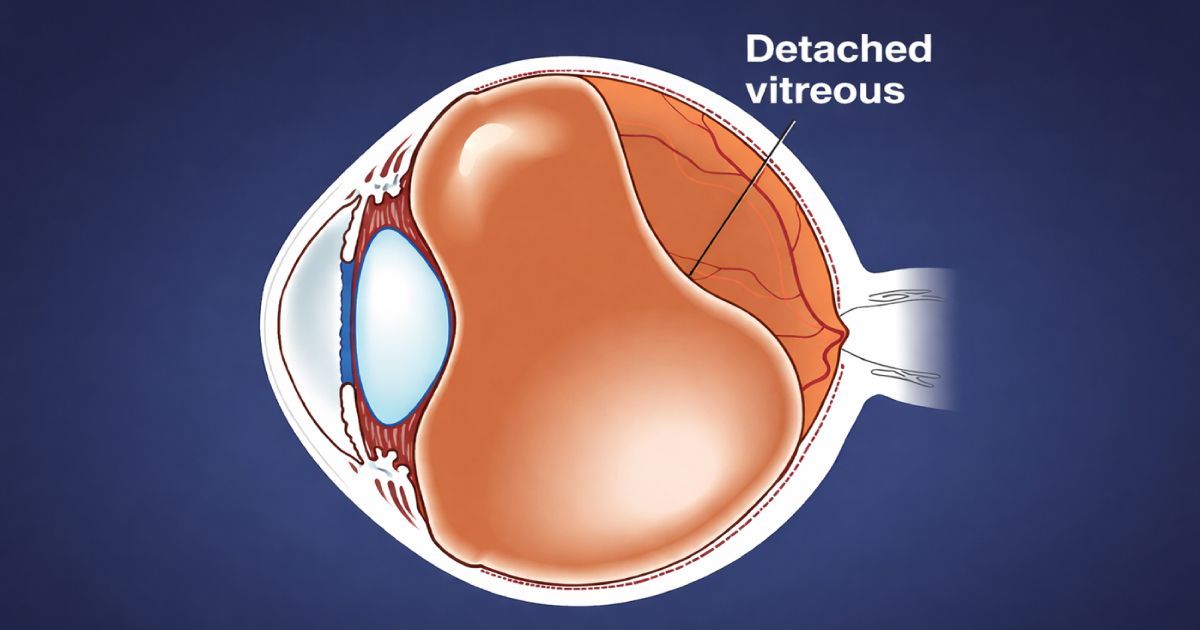
The exact cause of VSS is still unknown, but it is known to be a problem with how the brain processes what we see. Think of it like this: your eyes see the world, but your brain is what makes sense of it. In VSS, there's a mix-up in brain processing. Studies show that certain parts of the brain, like the visual cortex (which handles what we see), might be too active, while other parts that help filter out unimportant information might not be active enough. This imbalance messes up the brain's ability to "clean up" the visual signals, causing the constant "static."
It's also thought that VSS might involve problems with brain chemicals called neurotransmitters, such as serotonin and glutamate. These chemicals are crucial for how brain cells communicate, and if they're off balance, it can affect how we see and process sensory information. While many people develop VSS for no clear reason, sometimes it can start after certain events. Possible triggers include:
- Taking certain medications, especially some antidepressants.
- Periods of intense stress or emotional distress.
- Head injuries or concussions.
- Having migraines (though VSS is distinct from the visual "aura" some people get with migraines).
- Certain infections or surgical procedures.
- Using recreational drugs (even just once).
In some cases, VSS might even run in families, suggesting that genetics could play a role.
How Doctors Diagnose Visual Snow Syndrome
Diagnosing VSS relies mostly on carefully listening to a person's symptoms and making sure other conditions aren't causing them. This is important because VSS symptoms can sometimes look like other eye or brain problems.
The main symptom doctors look for is constant, tiny dots—a continuous "snow" or "static" across everything you see, which has been present for more than three months. These dots are usually black and white, but they can also flicker, be colored, or appear see-through. In addition to this core symptom, doctors will look for at least two of four other specific visual problems:
- Palinopsia: Seeing afterimages or trails of objects, like a faint "ghost" of a car that just drove by.
- Increased "Normal" Eye Phenomena: Such as seeing a lot of "floaters" (tiny specks or lines that drift in your vision), or noticing little bright dots when looking at a clear blue sky, or perceiving colored waves or clouds when your eyes are closed in the dark.
- Light Sensitivity (Photophobia): Being very bothered by bright lights, often causing people to avoid sunny places or brightly lit rooms.
- Night Blindness (Nyctalopia): Having a hard time seeing in dim light or at night, even if the eyes themselves are healthy.
To rule out other issues, doctors (including eye doctors and brain doctors) will perform a thorough check-up. This might involve comprehensive eye exams to ensure your eyes are healthy and rule out typical eye diseases. They might also order brain scans, such as an MRI or CT scan, to check for any physical problems in the brain that could be causing similar symptoms.
Read more about Visual Snow Syndrome from the Visual Snow Initiative.
Managing Visual Snow Syndrome
While there's currently no cure for Visual Snow Syndrome (VSS), a lot of progress has been made in managing symptoms and improving daily life. Treatment is highly personal and often includes a mix of therapies and lifestyle adjustments tailored to each individual.
One effective approach is brain and vision training. Neuro-optometric rehabilitation uses targeted exercises and sometimes special lenses to help the brain process visual information more clearly. Another helpful option is Mindfulness-Based Cognitive Therapy (MBCT). This technique teaches individuals how to calm their minds and focus attention, which can help reduce the brain’s reaction to the constant "static" and make the symptoms feel less overwhelming.
Many people with VSS find relief through special tinted lenses, such as FL-41 or amber/yellow shades. These can reduce light sensitivity, glare, and visual discomfort. Adjusting screen settings—using dark mode, lowering brightness, or adding blue light filters—can also make digital devices easier to use.
Since VSS often comes with sensory sensitivities, managing sensory input is important. Some people wear sunglasses indoors, use earplugs, or take breaks in quiet spaces. Stress management is also key—relaxation techniques, deep breathing, and doing enjoyable activities can make a big difference. And because sleep is so important for overall well-being, getting good rest can help keep symptoms from worsening.
While no medication works for everyone, some medicines like lamotrigine have shown promise. Others may help with related issues such as migraines or anxiety, which often accompany VSS.
Finally, finding community support can be incredibly helpful. Online groups and resources like the Visual Snow Initiative offer a space to connect with others, share experiences, and learn useful coping strategies.
The Takeaway
Visual Snow Syndrome is no longer a hidden condition. With growing awareness, clearer ways to diagnose it, and new ideas for treatment and management, people with VSS can now find understanding, support, and hope for a better life. If you think you or someone you know might have VSS, the most important step is to see your Urban Optiks eyecare professional and possibly a neurologist to get a proper diagnosis and discuss management options.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.