Graves' Disease and Its Impact on Eye Health

Read time: 4 minutes
Graves’ disease is an autoimmune condition that primarily affects the thyroid gland, leading to an overproduction of thyroid hormones—a condition known as hyperthyroidism. While it is best known for its systemic effects, Graves’ disease is also closely associated with a serious eye complication called Thyroid Eye Disease (TED), sometimes referred to as Graves’ orbitopathy.
This article provides a factual overview of Graves’ disease, its historical background, how it affects the eyes, current treatment options, and promising advances in care.
What Is Graves’ Disease?
Graves’ disease occurs when the body’s immune system produces autoantibodies that stimulate the thyroid-stimulating hormone (TSH) receptor, causing the thyroid to overproduce hormones. This excess hormone production speeds up the body’s metabolism, which can lead to weight loss, heat intolerance, tremors, rapid heartbeat, and anxiety.
It is the most common cause of hyperthyroidism, accounting for 60–80% of cases. The condition affects more women than men and typically develops between the ages of 30 and 50, though it can occur at any age.
Historical Context
Graves’ disease is named after Robert J. Graves, an Irish physician who first described the condition in 1835. At the same time, German physician Karl von Basedow independently described the same disease, which is why it is still called Basedow’s disease in some regions.
The connection between thyroid dysfunction and eye problems was noted early in medical history, but it wasn’t until the 20th century that researchers realized the eye symptoms were caused by a separate but related autoimmune reaction.
For more additional info on Graves’ disease, see the Mayo Clinic Q&A.
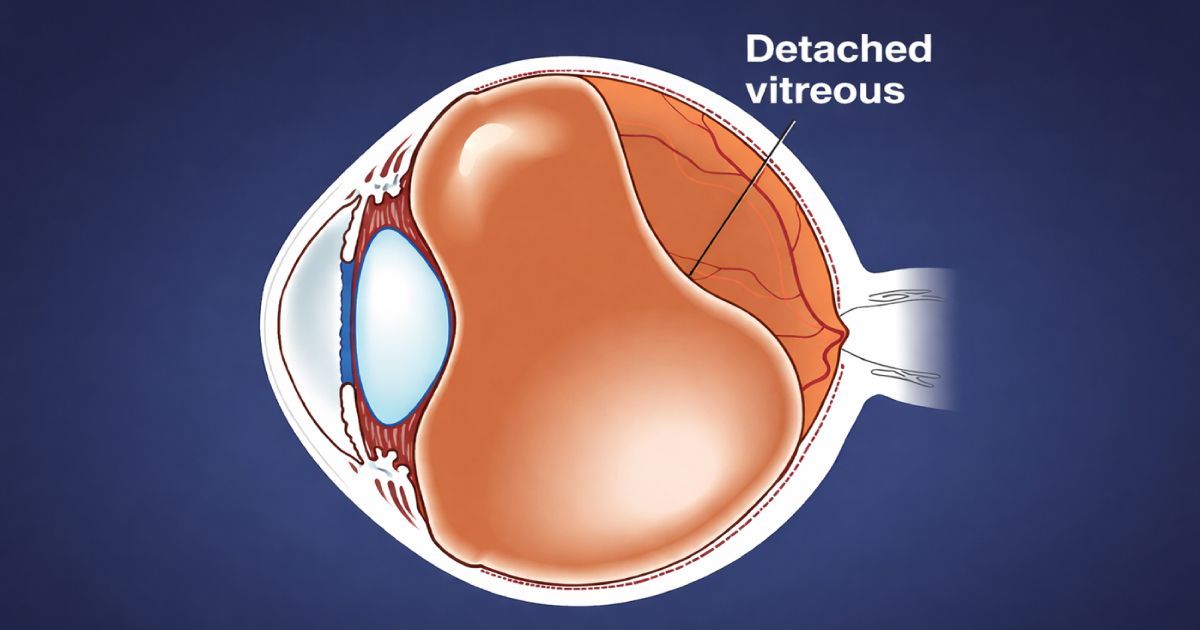
Thyroid Eye Disease (TED): The Ocular Component
Up to 50% of people with Graves’ disease develop some form of Thyroid Eye Disease, a condition in which the immune system attacks the tissues around the eyes, including muscles, fat, and connective tissue.
TED can develop before, during, or after the onset of hyperthyroidism, and in rare cases, it occurs even in people with normal thyroid function. Explore more about the TED connection from the American Thyroid Association
Common Symptoms of TED include:
- Bulging eyes (proptosis or exophthalmos)
- Redness and swelling
- Gritty or dry eye sensation
- Sensitivity to light (photophobia)
- Double vision (diplopia)
- Difficulty closing the eyes completely
- Eyelid retraction or a staring appearance
- In severe cases, optic nerve compression leading to vision loss
TED is typically divided into two phases: the active (inflammatory) phase, which lasts 6 to 24 months, and the inactive (fibrotic) phase, where the condition stabilizes but may leave behind structural changes.
Diagnosis and Monitoring
Diagnosing Graves’ disease and TED involves a combination of bloodwork, imaging, and eye exams. Thyroid function tests measure hormone levels (TSH, T3, and T4), while antibodies such as TRAb (thyroid-stimulating immunoglobulins) are often elevated.
For the eyes, evaluations may include:
- Exophthalmometry to measure eye protrusion
- Visual field and acuity testing
- Ocular motility assessment for double vision
- CT or MRI scans to assess orbital swelling or nerve compression
- OCT to monitor retinal and optic nerve health
Current Treatment Options
Treating Graves’ disease requires addressing both thyroid function and eye complications, often in coordination between endocrinologists and eye care professionals.
Systemic treatments for Graves’ disease include:
- Antithyroid medications
- Radioactive iodine therapy to reduce thyroid activity
- Thyroidectomy (surgical removal) in selected cases
These therapies stabilize hormone levels but do not directly treat the eyes.
Treatments for Thyroid Eye Disease may involve:
- Lubricating drops and ointments to ease dryness
- Corticosteroids (oral or IV) to reduce inflammation
- Selenium supplementation in mild, early cases
- Orbital radiation therapy for moderate-to-severe inflammation
- Strabismus surgery for double vision
- Orbital decompression surgery for severe bulging or optic nerve compression
- Eyelid surgery to restore function and appearance
Recent Advances in Treatment
A breakthrough therapy was introduced in 2020 with the FDA approval of teprotumumab, the first targeted treatment for active TED. This monoclonal antibody blocks the insulin-like growth factor-1 receptor (IGF-1R), which plays a role in the autoimmune process.
Clinical trials have shown that teprotumumab can reduce eye bulging, improve double vision, and decrease inflammation — offering a treatment that not only manages symptoms but also alters the disease course.
Future Directions in Care
Research continues into the immune mechanisms behind Graves’ disease and TED. Future treatments may include:
- Additional biologics targeting immune pathways involved in TED
- Gene-based therapies to address underlying autoimmune triggers
- Minimally invasive surgical techniques for orbital decompression and eyelid correction
- Predictive imaging using AI to forecast disease progression and treatment response
With deeper insight into molecular pathways, future care will likely move toward earlier intervention and more personalized treatment plans.
The Takeaway
Graves’ disease is a complex autoimmune disorder that can significantly impact both systemic health and eye function. The eye condition associated with it, Thyroid Eye Disease, can cause both cosmetic and vision-threatening changes.
The good news is that with early detection, advanced monitoring, and modern treatments like teprotumumab, patients have more options than ever before. At Urban Optiks Optometry, we use state-of-the-art diagnostic tools to track systemic-related eye changes and deliver personalized care.
If you have thyroid dysfunction or are experiencing symptoms that affect your eyes, schedule a comprehensive eye exam to protect your vision and overall well-being.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.